Background
VEXAS (Vacuoles, E1 Enzyme, X-Linked, Autoinflammatory, Somatic) syndrome is an autoinflammatory monogenic disease caused by inactivating somatic mutations in the UBA1 gene and characterized by heterogenous systemic auto-inflammation and progressive hematologic manifestations. Its management is not consensual but often include biologic DMARDs or azacitidine in case of association with myelodysplastic syndrome. Prognosis appears to be poor, with substantial morbidity and mortality mainly caused by infection. The aim of this study was to describe the spectrum of serious infectious complications and their potential risk factors in VEXAS patients.
Methods
We conducted a retrospective multicenter study including patients with genetically proven VEXAS syndrome from the French VEXAS registry. Episode of serious infections (defined as an infection leading to hospitalization and/or intravenous infectious treatments and/or death) were described, and their risk factors analyzed with multivariable Cox proportional hazard models.These patients were compared to a cohort of 50 VEXAS patients without serious infection after at least one year of follow-up since diagnosis.
Results
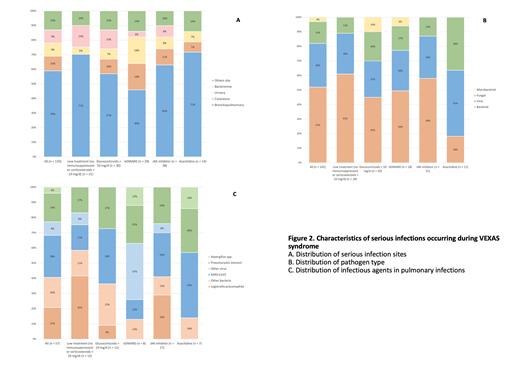
Seventy-four patients (99% male, median [IQR] age at VEXAS onset of 68 [63-75] years) with 133 serious infections were included. Infections occurred despite anti-infective prophylaxis in 46% of cases. The main immunosuppressive drugs received at the time of infection were JAK inhibitors (29%), biologics (21%) and azacitidine (11%), while 16% of infections occurred without treatment (no immunosuppressant or corticosteroids ≤ 10 mg/d).The most common sites of infection were lung (59%), skin (10%) and urinary tract (9%). Microbiological confirmation was obtained for 76%: 52% bacterial, 30% viral, 15% fungal and 3% mycobacterial. Among pulmonary infections, the main infectious agents were SARS-CoV-2 (28%), Legionella pneumophila (21%) and Pneumocystis jivoreci (19%) (Figure 1). Invasive fungal infections accounted for 11% of all infections. Nearly 20% of pulmonary infections occurred in the absence of treatment with a high prevalence of L. pneumophila (42%) and P. jivoreci (17%) infections. In multivariate analysis, age >75 years (HR [95%CI] 1.91 [1.05-3.47]), p.Met41Val mutation (2.44 [1.05-5.63]) and arthralgia (2.03 [1.16-3.56]) were associated with the risk of first serious episode of infections. Among treatments, JAK inhibitors were the most associated with serious infections (4.51 [2.19-9.26] compared to biologics and azacitidine. After a median follow-up of 4.4 [2.5-7.7] years, 27 (36%) patients died including 15 (56%) due to serious infection.
Conclusion
VEXAS syndrome is associated with a high incidence of serious infections especially in patients carrying the p.Met41Val mutation. The high frequency of atypical infections such as legionellosis and invasive fungal infections in patient without immunosuppressive treatment might suggest an intrinsic immunodeficiency of the disease. JAK inhibitors, used as first-line treatment, are particularly at risk of serious infections occurring early after initiation.
Disclosures
Heiblig:Jazz Pharmaceuticals: Honoraria; AbbVie: Honoraria; Pfizer Inc.: Honoraria; Astellas: Honoraria; Servier: Honoraria. Fenaux:Janssen: Consultancy, Honoraria, Research Funding; AbbVie: Consultancy, Honoraria, Research Funding; Jazz: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Research Funding; Bristol Myers Squibb: Consultancy, Honoraria, Research Funding; French MDS Group: Honoraria. Comont:Novartis: Honoraria, Speakers Bureau; BMS: Consultancy, Speakers Bureau; Amgen: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal